Israel Journal of Health Policy Research: Integration of advanced practice providers into the Israeli healthcare system
Integration of advanced practice providers into the Israeli healthcare system | Israel Journal of Health Policy Research | Full Text
Many countries around the world have integrated various types of Advanced Practice Providers (APPs) into their healthcare systems. The main motivating factors for recognizing and developing APPs worldwide include physician shortages and the need for improved access or delivery (US, France, Belgium, Scotland, Switzerland), reduced residency hours (US, UK), shortages in underserved regions (US, Canada, Finland, Australia), and cost containment (Germany, Netherlands, UK, US). Israel is experiencing a shortage of physicians in peripheral geographic regions and in critical medical specialties. Recent by-laws approved by the Knesset (Parliament), combined with Israel Ministry of Health (MOH) policies, have thus far been unable to fully address the shortages. To understand the potential contribution of APPs in Israel, we evaluated the international historical foundations and development of APP roles. We assessed how APPs have impacted healthcare in other countries by analyzing public data and published international research about APP education, safety, quality of care, motivators, barriers, and impact. We found that APPs are recognized in dozens of countries, and have similar scopes of practice, graduate level education requirements (in developed countries), and clinical training. At the same time, there is wide variability among countries in the actual function and independence of the advanced practice nurse (APN), particularly the nurse practitioner (NP). APPs have been established as cost effective, safe healthcare providers who improve healthcare access. Israel has begun to introduce APPs, specifically NPs, in a variety of fields, including geriatrics, palliative care and diabetic care. We recommend a rapid expansion of existing and new APP roles into the Israeli healthcare system based on evidence and the recommendations of international evaluations by non-government organizations. By shifting the education to a university setting, mirroring successful, evidence-based, and established APP models found internationally, Israel could lessen the projected Israeli physician shortage, improve healthcare access in specific areas, and bolster existing resources towards a larger and richer pool of healthcare providers in Israel.
Our Latest Blogs
25 June 2023
Medical Checklist for Gap Year Students It's probably safe to say that the Gap year packing list your child received did not include a medical supplies checklist. There are many reasons to give your kids some medical supplies and medicines before the...
31 October 2021
You have decided to make your Aliyah and currently take prescription medications. How can you continue with your medication regimen in Israel? How can you ensure that your medications are available in Israel and how do you communicate the need for th...
17 October 2021
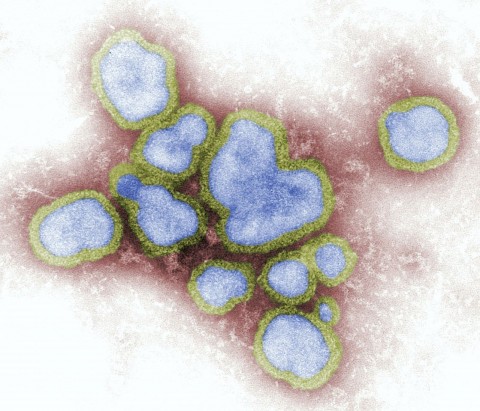
During the Coronavirus pandemic, many people have been worried about the upcoming Flu season. But to everyone’s surprise, the numbers in the southern hemisphere were the lowest they have been in a long time. “Never in my 40-year career have we ever s...
EMA Care in the News
05 September 2021
Medical Care during the Holidays can be tricky in Israel especially if you do not speak Hebrew. During the holidays, many medical offices and hospitals are operating on Shabbat mode. Shabbat mode means that personnel is cut to minimum staffing, many ...
19 July 2021
Over the years, we've been approached by people who've asked us about different kinds of diets and food plans. Intermittent fasting has become very popular over the last few years. It is a method of dieting that restricts the amount of time you are a...
11 July 2021
Telemedicine is a great option for caring for geriatric populations in Israel. This is especially true during the Covid-19 pandemic. Over the years, we’ve had many clients who care for their older, dependent parents. Take our clients, the A fam...